Introduction
The Apgar score might sound like something out of a sci-fi movie, but it’s actually a lifesaver in the world of newborn health! Developed by Dr. Virginia Apgar in 1952, this scoring system provides vital information about a baby’s well-being right after birth. Think of it as a newborn’s first report card—except there are no grades for art or gym.
So, what’s the big deal about the Apgar score? Well, it evaluates five critical criteria to see how well a baby is transitioning to life outside the womb. These criteria include Appearance, Pulse, Grimace response, Activity, and Respiration. Each aspect is given a score from 0 to 2, with a perfect score being 10. However, scoring a perfect 10 is as rare as finding a unicorn, because most babies arrive with some blue-tinted extremities!
The stakes are incredibly high in those first moments. A low score can indicate that a baby may need immediate medical attention. This quick assessment helps healthcare professionals make swift decisions about necessary interventions. In this guide, we will dissect the Apgar score, uncover its components, and discuss its significance.
What do those numbers really mean for your little one? Are they just a way to impress your friends at brunch, or do they carry real weight in the world of healthcare? Join us as we break down the nuances of the Apgar score and what it signifies for the health of newborns. You’ll leave equipped with knowledge and perhaps a few witty anecdotes to share at your next gathering!

Components of the Apgar Score
Overview of the Apgar Score
The Apgar score is a quick test performed on newborns to evaluate their health immediately after birth. This scoring system was developed by Dr. Virginia Apgar, an anesthesiologist, in 1952. She created this tool to standardize the evaluation of infants, ensuring no baby would slip through the cracks during those critical moments.
The primary purpose of the Apgar score is to assess how well a newborn is adapting to life outside the womb. It provides healthcare professionals with vital information on whether immediate medical intervention is necessary. The score is based on five criteria: Appearance, Pulse, Grimace response, Activity, and Respiration. These criteria give a snapshot of the newborn’s overall condition, allowing for timely and appropriate medical responses. The Apgar score has become a cornerstone in neonatal care, as it significantly impacts early health interventions.

The Five Criteria
Appearance (Skin Color)
The first criterion, Appearance, evaluates the newborn’s skin color, which can reveal a lot about their oxygen levels. Scoring is straightforward: a score of 0 is given if the baby appears blue or pale all over, indicating possible oxygen deprivation. A score of 1 is assigned if the body is pink but the extremities remain blue, often seen in healthy newborns during the transition to breathing air. A perfect score of 2 is awarded when the baby is entirely pink, a sign that oxygenation is on point. Monitoring the skin color helps determine whether the baby is breathing effectively and receiving enough oxygen.
Speaking of keeping an eye on your little one, a Baby Monitor with Camera can be a lifesaver! Imagine being able to check in on your baby from another room. You can sip your coffee while ensuring they’re safe and sound. It’s like having a personal security system for your precious bundle of joy!

Pulse (Heart Rate)
Next up is Pulse, which measures the newborn’s heart rate. A score of 0 indicates no heartbeat, which is alarming. If the heart rate is below 100 beats per minute, the baby scores a 1. A score of 2 is given for a heart rate above 100 bpm, which is reassuring. A healthy heart rate is crucial for circulation and overall well-being, making this criterion vital in assessing a newborn’s immediate health status. Low heart rates can signal a need for urgent medical attention or resuscitation.

Grimace Response (Reflexes)
Grimace Response evaluates the baby’s reflexes and responsiveness to stimuli, providing insights into neurological function. A score of 0 means there’s no response to stimulation, which raises concerns. A score of 1 is assigned for a grimace in response to suctioning or stimulation. The highest score of 2 is given when the baby cries, coughs, or sneezes, showing robust reflexes. This criterion is essential for understanding how well the baby is neurologically attuned to its environment, which can indicate potential complications.

Activity (Muscle Tone)
Activity assesses muscle tone, which can reflect the baby’s physical health. A score of 0 is awarded if the baby appears limp, suggesting severe distress. A score of 1 is given for some flexion of the arms and legs, indicating moderate muscle tone. The best score of 2 is awarded for active movement, showing that the baby is strong and responding well. Active movement is a positive sign, suggesting that the baby is adjusting well to the new environment, and it can guide healthcare providers in their observations.

Respiration (Breathing)
Finally, Respiration evaluates the baby’s breathing effort. A score of 0 indicates no breathing, a critical situation requiring immediate intervention. If the newborn exhibits weak or irregular breathing, they score a 1. A 2 is given for a strong, robust cry, which is a reassuring sign of effective respiratory function. Establishing normal breathing is crucial for the newborn’s survival and overall health, emphasizing the importance of this last criterion.

In summary, the Apgar score consists of these five criteria, each contributing to a comprehensive picture of a newborn’s health. The total score ranges from 0 to 10, with higher scores indicating better health and fewer immediate concerns. Understanding these criteria can help parents and caregivers appreciate the quick assessments performed on their newborns and the importance of timely medical intervention when necessary.
Understanding the Scores
The Apgar score ranges from 0 to 10. It’s a quick snapshot of a newborn’s health at one and five minutes after birth. Let’s break it down!
A score of 7-10 is considered normal. Babies scoring in this range are generally doing well. They’re pink, have a good heartbeat, and are breathing strong. These little ones are ready to take on the world!
Scores between 4-6 indicate a moderate level of concern. Babies in this range may need some assistance. Common interventions include supplemental oxygen or suctioning of the airways. It’s like giving them a helping hand to adjust to their new environment.
Now, if a baby scores 0-3, that’s a serious red flag. This score suggests the newborn is in distress and needs immediate medical attention. A team of healthcare providers springs into action, ready to perform resuscitation or other critical interventions.
In summary, understanding these score ranges can help parents and caregivers gauge their newborn’s immediate health status. The Apgar score isn’t just a set of numbers; it’s a lifeline in those first moments of life.

Factors Affecting the Apgar Score
Several factors can influence a baby’s Apgar score. Let’s look at both maternal and infant factors.
Starting with maternal factors, anesthesia during labor can impact the score. Medications like epidurals might delay a baby’s response post-birth. Complications such as prolonged labor or infections can also play a role. It’s essential for healthcare providers to consider these elements when assessing the score.
Now, let’s shift to infant factors. Prematurity is a significant player here. Preterm infants often struggle to adapt and may score lower on the Apgar scale. Congenital conditions can also affect the score. These conditions might impact respiratory function or overall muscle tone.

Birth trauma is another factor to consider. If a baby experiences physical stress during delivery, it can reflect in their Apgar score. This might include bruising or fractures, which can complicate their transition.
In conclusion, both maternal and infant factors contribute to the Apgar score. Understanding these influences is crucial for interpreting the results accurately. Remember, the Apgar score is just one tool in assessing a newborn’s health.
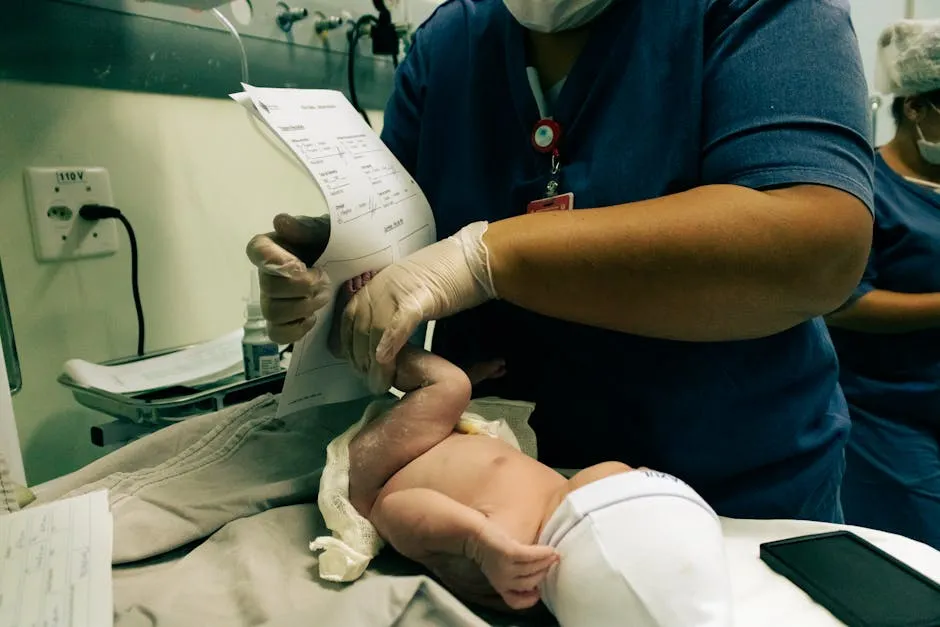
Documentation and Communication
Accurately recording the Apgar scores is paramount. These scores are not just numbers; they represent a newborn’s immediate health status. If healthcare professionals misplace or overlook these figures, crucial time may be lost in administering needed interventions. Imagine a baby who needs oxygen but gets overlooked because of a scribbled score. Yikes!
The Apgar score plays a significant role in guiding medical interventions. For instance, scores below 7 may prompt immediate action, like oxygen support. A score of 4-6 suggests that the baby needs some assistance, while anything below 4 signals a critical situation. This means swift decisions must be made. Doctors and nurses are like superheroes in this scenario, armed with numbers to save the day.
Moreover, effective communication among healthcare providers is essential. When a baby scores low, the information must flow seamlessly between the delivery room and the neonatal unit. Everyone needs to be on the same page. This ensures that every medical team member knows the necessary steps to take. A score of 5 at one minute followed by a score of 8 at five minutes? That tells a story of improvement worth celebrating!

And speaking of celebration, new parents often find themselves needing a reliable Diaper Bag Backpack. It’s perfect for carrying all those baby essentials while keeping your hands free for all the cuddles! Trust me, you’ll need that extra arm for all the hugs.
In summary, accurate documentation and clear communication regarding Apgar scores are crucial for ensuring the best possible care for newborns. These scores inform urgent medical decisions and contribute to the overall safety of the little ones during their initial moments in the world. Every second counts, and those numbers can make all the difference!

Limitations and Critiques of the Apgar Score
Common Misconceptions
The Apgar score is often misunderstood. One common misconception is that it predicts long-term outcomes. Spoiler alert: it doesn’t! While the score provides a snapshot of a newborn’s condition, it doesn’t foresee future health issues. Many babies with low scores go on to thrive, proving that first impressions aren’t everything.
Another area of confusion lies in race and skin color. Some believe that darker skin tones may lead to lower scores due to subjective interpretations of color. This has raised eyebrows and sparked discussions in the medical community. The reality is that the Apgar score’s components can sometimes misrepresent a baby’s health based on their pigmentation. It’s essential to recognize and correct these biases, ensuring that every baby gets the fair assessment they deserve.
Proposed Improvements and Alternatives
In response to the Apgar score’s limitations, the medical community is buzzing with ideas for improvement. One such suggestion is the Combined-Apgar score, which takes the original scoring system and adds more components for a more nuanced assessment. This new score can reach a maximum of 17 points, providing a more detailed picture of a newborn’s health.
Ongoing research aims to enhance the Apgar scoring system further. Discussions are focusing on how to integrate technological advancements, like pulse oximetry, into the evaluation process. This could reduce subjectivity and provide a more accurate assessment of a newborn’s condition. The goal? To ensure that every baby gets the best possible start in life, regardless of their background or circumstances.
And while we’re talking about enhancements, don’t forget about your little one’s comfort! A cozy Baby Swaddle Blanket can help them feel secure and snug, mimicking the womb experience. It’s a win-win for both baby and parent!
In conclusion, while the Apgar score remains a vital tool in neonatal care, acknowledging its limitations and striving for improvements can help ensure fair and effective assessments for all newborns.
Conclusion
The Apgar score is more than just a set of numbers—it’s an essential tool in neonatal care. This quick assessment helps healthcare providers gauge a newborn’s health immediately after birth. Scoring is based on five criteria: Appearance, Pulse, Grimace response, Activity, and Respiration. Each is crucial for understanding how well a baby is adjusting to life outside the womb.
While a perfect score of 10 is rare—think of it as spotting a unicorn—scores of 7-10 generally indicate good health. Conversely, lower scores signal potential challenges. It’s important to note that the Apgar score is not a crystal ball for predicting a baby’s future health; rather, it provides immediate insights that can guide critical interventions.
As we continually refine our approaches to neonatal care, acknowledging the Apgar score’s strengths and limitations is vital. Parents should understand this scoring system, empowering them during those first precious moments with their newborn. After all, knowledge is power, especially when it comes to the health of your little one.
By familiarizing themselves with the Apgar score, parents can better advocate for their baby’s needs. So, whether you’re awaiting your little bundle of joy or simply brushing up on parenting tips, remember that this score is a valuable part of assessing newborn health. Embrace the knowledge, and feel confident in navigating those early days!

FAQs
What is the highest possible Apgar score?
The highest Apgar score is 10, but it’s rare. Most babies score lower due to temporary conditions, like bluish extremities. A score of 10 indicates optimal health, with no signs of distress.
How often is the Apgar score assessed?
The Apgar score is typically assessed at 1 minute and again at 5 minutes after birth. If scores remain low, healthcare providers may continue assessments every 5 minutes until the baby’s condition stabilizes.
Can a baby with a low Apgar score be healthy?
Yes! Many babies with low Apgar scores can recover quickly with appropriate care. It’s crucial to remember that the score reflects a snapshot of health at a specific time, not a definitive measure of long-term outcomes.
What should I ask my healthcare provider about the Apgar score?
Consider asking: What was the Apgar score for my baby?What does this score mean for my baby’s health?Are there any interventions needed based on the score?How will the care team monitor my baby moving forward?
Are there recent changes to the Apgar scoring system?
While the traditional Apgar scoring system remains widely used, discussions about enhancements, like the Combined-Apgar score, are ongoing. This alternative aims to provide a more nuanced assessment, especially for preterm infants requiring additional support.
And while you’re preparing for your little one’s arrival, consider investing in a First Aid Kit for Babies. You never know when a little boo-boo might happen, and it’s always better to be prepared!
Please let us know what you think about our content by leaving a comment down below!
Thank you for reading till here 🙂
For more insights on how data influences healthcare practices, check out this article on statistics for healthcare professionals on workplace safety 2024.
All images from Pexels